Understanding Fungal Acne. What is Fungal Acne?

Warning: This submit could include affiliate hyperlinks. As an Amazon Associate, I can earn from qualifying purchases.
Fungal acne is a skin condition where an overabundance of yeast manifests, leading to folliculitis—an infection deep within the minuscule hair follicles. This infection gives rise to small red bumps or lesions. While fungal acne can surface anywhere, it’s most frequently observed along the chin, forehead, hairline, nose’s flanks, arms, upper back, and shoulders. Known by its more scientific terms, Pityrosporum folliculitis or Malassezia folliculitis, it stems from an overgrowth of Malassezia yeast.
Fungal acne typically materializes as clusters of uniform papules (spots), resembling whiteheads, and often incites itching. Although it mirrors bacterial acne visually, it’s fundamentally distinct. Bacterial acne stems from oil and dead skin cells clogging the pores, whereas fungal acne is rooted in yeast infection within the follicles. Furthermore, while bacterial acne can manifest as blackheads, pustules, or cysts, fungal acne doesn’t take such forms. Misidentifying fungal acne and treating it with bacterial acne products can exacerbate the condition, which is why professional diagnosis is essential, preferably by a dermatologist like Dr. Michele Green.
What Triggers Fungal Acne?
Fungal acne arises due to yeast proliferation on the skin, specifically the Malassezia yeast, which coexists with bacteria on the skin’s surface. Typically, a balance between yeast and bacteria maintains skin health, but when this balance tips—such as when bacteria are diminished due to antibiotics—yeast overgrowth can occur, leading to folliculitis and fungal acne. This yeast thrives in warm, moist environments, making such conditions a key risk factor for fungal acne development. The yeast also feeds on skin’s natural oils, meaning those with oily skin or areas where oil production is high are more prone to outbreaks.
Risk Factors Associated with Fungal Acne
Numerous factors heighten the risk of developing fungal acne, many of which are preventable through lifestyle adjustments. Warm, humid environments are particularly conducive to yeast growth. Research indicates that fungal acne is more prevalent in hot, humid regions like the Philippines compared to cooler climates like the United States. Moisture trapped in sweaty clothing can further fuel yeast growth, especially when clothes are worn again before washing. Opting for loose, breathable clothing when in warm environments is advisable, as tight garments are more likely to trap moisture and contribute to fungal proliferation.

Another contemporary risk factor is the use of face masks, particularly during the COVID-19 pandemic. Masks, especially those made from non-breathable materials, can trap moisture from breath, creating a favorable environment for yeast growth along the nose and chin. Swapping masks frequently or choosing those made from more breathable materials like cotton can mitigate this risk.
Best Practices for Treating Fungal Acne
Navigating the complexities of fungal acne treatment can be challenging. If you suspect an outbreak, it’s crucial to consult a certified dermatologist, such as Dr. Michele Green. Dr. Green can accurately assess the condition and recommend a tailored skin care regimen. Her expertise in treatments—from cleansers to moisturizers and even oral antibiotics—ensures that you receive care suited to your skin type, be it dry, combination, or oily.
Medications and Their Role in Fungal Acne
An imbalance between skin bacteria and yeast can also result from certain medications. For instance, oral antibiotics intended to eliminate harmful bacteria can inadvertently diminish the beneficial bacteria on your skin. This creates an imbalance, allowing Malassezia yeast to proliferate, which can trigger fungal folliculitis. Using skin care products rich in oils like coconut oil can further exacerbate the condition by feeding the yeast and clogging pores.

Identifying Fungal Acne
Distinguishing fungal acne from bacterial acne is vital since the treatments for each differ significantly. While traditional acne treatments like salicylic acid cleansers might help clear clogged pores, they are often ineffective against fungal acne. Consulting a dermatologist like Dr. Green ensures the most appropriate treatment plan. At home, there are a few key differences that can help in distinguishing between the two:
- Location: Fungal acne can appear on the chest, arms, shoulders, and upper back, whereas bacterial acne typically remains confined to the face.
- Size Consistency: Fungal acne presents as uniform-sized clusters, while bacterial acne spots vary in size.
- Clustering: Bacterial acne often appears randomly, but fungal acne forms in clustered areas.
- Itching: Unlike bacterial acne, fungal acne is frequently itchy, making it easier to identify.
Does Fungal Acne Resolve on Its Own?
Fungal acne rarely disappears without intervention. As a yeast infection, it requires specific treatment to eliminate the overgrowth and restore balance in the skin’s ecosystem. Without proper care, fungal acne can persist for months. With an accurate diagnosis, dermatologists like Dr. Green can effectively treat fungal acne and provide lasting solutions.

Treating Fungal Acne
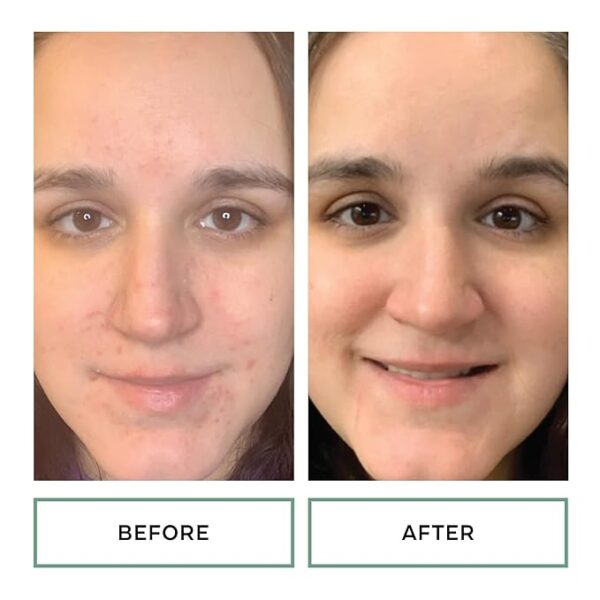
There are numerous treatments for fungal acne, ranging from topical antifungal creams to oral medications. If you suspect you’re dealing with fungal acne, a consultation with Dr. Michele Green can help determine the most effective treatment plan. Diagnosing fungal acne accurately is crucial, as using conventional acne treatments could worsen the condition.
Skin Care Tips for Fungal Acne
For those unfamiliar with fungal acne, there’s a risk of mistaking it for traditional acne and using products designed for acne vulgaris. However, these products are not only ineffective against fungal acne but could worsen the condition. It’s essential to seek a proper diagnosis. Dermatologists like Dr. Green can help tailor a treatment plan, often involving antifungal products such as Nizoral or Clotrimazole creams, dandruff shampoos like Selsun Blue, or oral medications like Fluconazole.

To effectively treat fungal acne, restoring the balance between yeast and bacteria on the skin is essential. Here’s a breakdown of various treatments, including topical and oral medications, as well as home remedies:
Ketoconazole
Ketoconazole is a widely used antifungal treatment available as a topical cream or shampoo. A key ingredient in Nizoral Shampoo, it has proven to be highly effective against fungal acne. In a 2020 study, nearly 50% of participants using a 2% ketoconazole cream saw a marked improvement in their fungal acne. This treatment is gentle on the skin and can be combined with oral medications if necessary.
Oral Fluconazole
Fluconazole is a prescription oral antifungal used when topical treatments don’t fully address fungal acne. Typically paired with a ketoconazole topical cream, fluconazole can clear fungal acne in one week with a 100mg daily dose or over three weeks with a 200mg daily dose.
How to Use Nizoral for Fungal Acne
Nizoral Shampoo, containing ketoconazole, treats fungal acne by reducing yeast growth on the skin. Apply it as a body wash during your shower, letting it sit on your skin for at least 30 seconds before rinsing. During an active outbreak, use Nizoral every other day. Once the infection clears, use it weekly to prevent recurrence and maintain clear skin.
At-Home Treatments for Fungal Acne
Improving hygiene is key to reducing fungal acne. Showering more frequently, especially after workouts, helps remove sweat that creates a moist environment for yeast. Incorporating dandruff shampoos like Nizoral or those containing selenium sulfide in your routine can reduce yeast on the body. Loose clothing during exercise and breathable face masks can also help. Over-the-counter antifungal creams containing ketoconazole or clotrimazole can be used to treat the condition at home.
Treating Fungal Acne on the Face
Fungal acne on the face can be addressed with prescription topical creams applied twice daily or oral medications for more severe cases. Showering more often, particularly after physical activities, can help wash away yeast and reduce outbreaks.
Treating Fungal Acne on the Forehead
The forehead and hairline are common areas for fungal acne. Topical treatments containing ketoconazole, butenafine, or clotrimazole, along with oral medications like itraconazole, are effective. Additionally, applying dandruff shampoo to the forehead and leaving it on for 30 seconds before rinsing can help eliminate fungal acne in this area.
Natural Remedies for Fungal Acne on the Face
If you prefer natural treatments, start by reducing your intake of sugary, carbohydrate-heavy foods since yeast thrives on these. Use oil-free skincare products, including a salicylic acid-based cleanser and oil-free moisturizer. If your fungal acne persists after three weeks of home treatment, consult a dermatologist like Dr. Green for further evaluation and treatment options, including topical creams, dandruff shampoos, or prescription oral medications.
By understanding these options and making adjustments to your skincare routine, fungal acne can be effectively treated and prevented.
How to Treat Pityrosporum Folliculitis on the Arms and Back
Pityrosporum folliculitis, also known as fungal acne, can commonly affect the arms and back, especially in environments where moisture is trapped against the skin. This condition is often triggered by wearing tight clothing in hot, humid conditions or staying in sweaty clothes after exercise. To prevent fungal acne outbreaks, you can adopt the following habits:
- Shower Regularly: Ensure you shower frequently, especially after sweating, to wash away the yeast that may have accumulated on your skin.
- Change Clothes Promptly: After a workout, change out of sweaty clothes immediately to prevent moisture from trapping yeast on your body.
- Wear Loose, Breathable Clothing: Opt for loose clothing that allows airflow and reduces moisture buildup on the skin.

To treat fungal acne on the arms and back, you can use:
- Topical antifungal creams: Look for creams containing ketoconazole, butenafine, or clotrimazole.
- Oral antifungal medications: In severe cases, prescription oral antifungals can be used to treat the condition more effectively.
Is Benzoyl Peroxide Good for Fungal Acne?
Benzoyl peroxide is a popular treatment for traditional bacterial acne because it works as an antimicrobial, killing bacteria and unclogging pores by exfoliating the skin. However, fungal acne is caused by an overgrowth of Malassezia yeast, not bacteria. As a result, benzoyl peroxide is not an antifungal treatment and is not effective against fungal acne.
While it doesn’t treat the root cause of fungal acne (yeast), benzoyl peroxide can still help reduce excess oil and unclog pores, which may prevent the yeast from thriving. However, for a more effective solution, antifungal treatments are recommended.
What is Good for Fungal Acne?
The most effective treatments for fungal acne focus on addressing the yeast overgrowth. Commonly recommended products include:
- Nizoral Shampoo or Cream (contains ketoconazole): Applying it as a topical treatment can help eliminate yeast on the skin.
- Mycelex Antifungal Cream (contains clotrimazole): This antifungal cream is also effective for treating fungal acne.
- Oral antifungal medications: For severe cases, oral antifungals like itraconazole or ketoconazole can be taken for one to three weeks to treat the condition from the inside out.
How to Prevent and Maintain Fungal Acne
To prevent fungal acne from recurring, it’s essential to control the environmental conditions that contribute to yeast overgrowth. Regular use of antifungal body washes or dandruff shampoos can be beneficial. Consider using:
- Nizoral Shampoo or Selsun Blue: These contain ketoconazole or selenium sulfide, which reduce yeast on the skin. Use them as a body wash once or twice a week, applying the shampoo to your skin, letting it sit for 30 seconds, and then rinsing it off.
Incorporating this routine into your skincare regimen can help keep fungal acne under control and prevent future outbreaks.